A cataract describes a lens that becomes progressively opaque. The lens is normally clear and serves to help focus light within the eye like the lens of a camera. When the lens becomes opaque, the vision declines like a windshield being covered gradually with snow. Cataracts can be focal or diffuse and can cause insignificant vision limitation or be completely blinding depending on their stage. Many cataracts are static and do not progress. Diabetic cataracts often progress very rapidly which can cause some secondary sequela that can be devastating and affect vision prognosis.
Diabetic Cataract Cause
Diabetic cataracts are osmotic cataracts that occur secondary to a disruption in normal lens metabolism. Since the lens does not have a blood supply, its energy needs are met via anaerobic glycolysis and glucose is able to diffuse across the lens capsule into and out of the lens freely. Whenever there is an abundance of glucose the anaerobic glycolysis pathway is overwhelmed, and an enzyme known as aldose reductase causes glucose to break down into fructose and sorbitol. Sorbitol is an alternate sugar that is unable to get back out of the lens and as a result, an influx of water flows into the lens causing damage to the lens cells and swelling of the lens. Clinically this results in what we see as a rapidly progressing cataract.
Who gets diabetic cataracts?
Most dogs with diabetes will develop cataracts within the first 1-2 years of their diagnosis. In most cases diabetic cataracts progress rapidly (days to weeks) but in some cases they can progress much more slowly or may not develop at all. Diabetic dogs with poor glucose control may suffer from more rapid progression however having “good” control of diabetes does not prevent cataract formation in many pets.
What about cats?
Cats do not typically develop diabetic cataracts due their lack of significant amounts of the enzyme aldose reductase. The lack of this enzyme means they do not break glucose down into fructose and sorbitol and therefore the osmotic cataracts do not develop.
Are any medical treatments available?
There is a medication on the horizon, not yet commercially available, that may be able to prevent cataract formation in our diabetic patients. It is an aldose reductase inhibitor which would inhibit the enzyme necessary for production of sorbitol and therefore prevent the subsequent osmotic effect it has within the lens. This medication is a preventative only and does not result in dissolution or treatment of cataracts once they develop.
What are the stages of cataract formation?
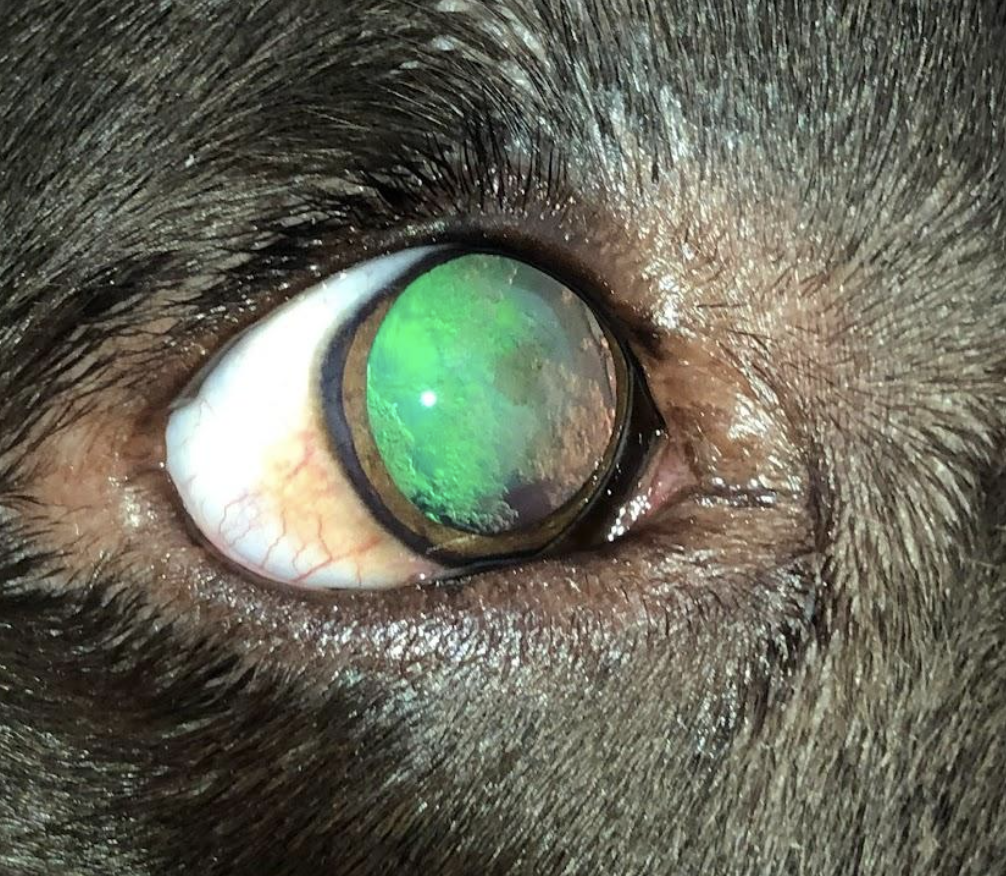
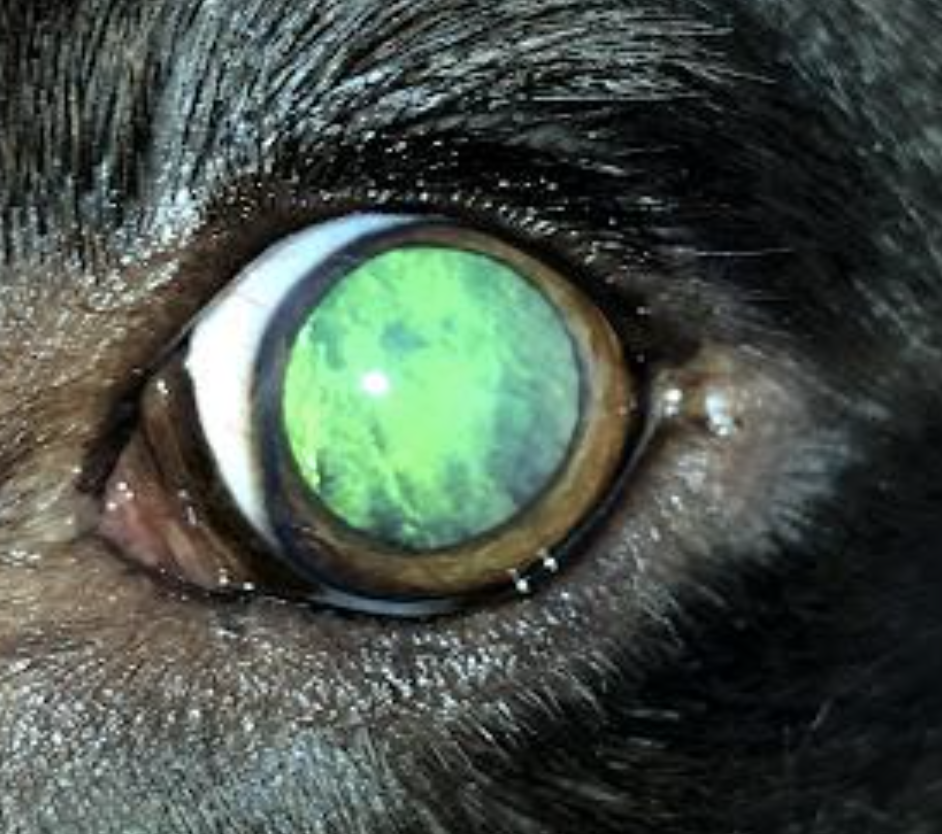
Cataracts are typically graded or staged based on their degree of opacity within the lens. This can most easily be determined by performing retro-illumination. Retro-illuminations allows us to see the reflection of the tapetum and then the degree of interference of that tapetal reflection to help determine the amount of cataract present.
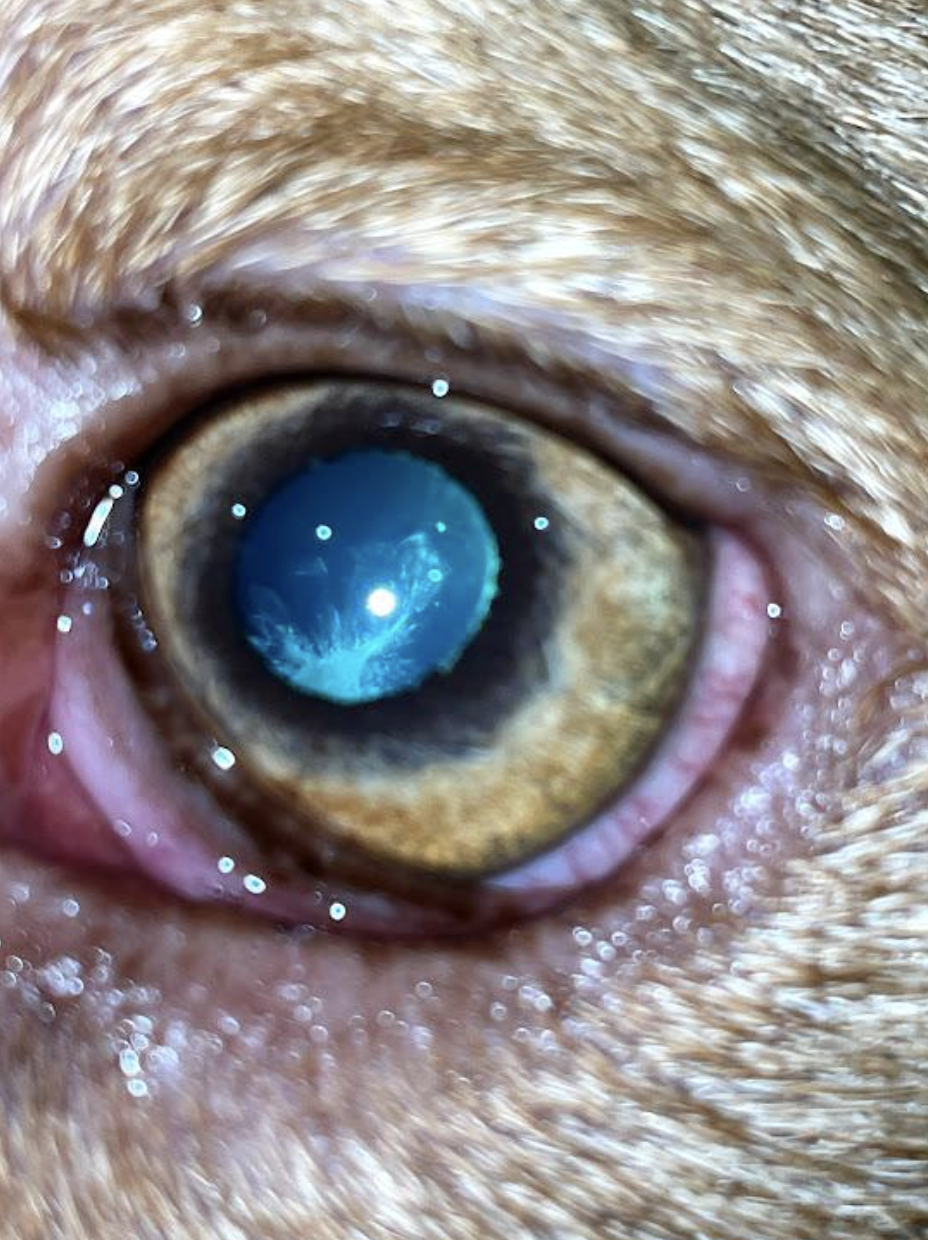
The earliest stage of cataract is the incipient stage. In this early stage the cataract is occupying 10% or less of the lens volume. This stage of cataract is typically considered clinically insignificant and does not require treatment. The likelihood of progression and timeline depend on the location of the cataract within the lens, age, breed, and cause of the cataract.
Immature cataracts are a much broader category and include cataracts between 10-99% of the lens being occupied by cataract. As you can imagine, the degree of vision limitation in the early stages is minor compared to the near blindness as cataracts advance toward maturity.
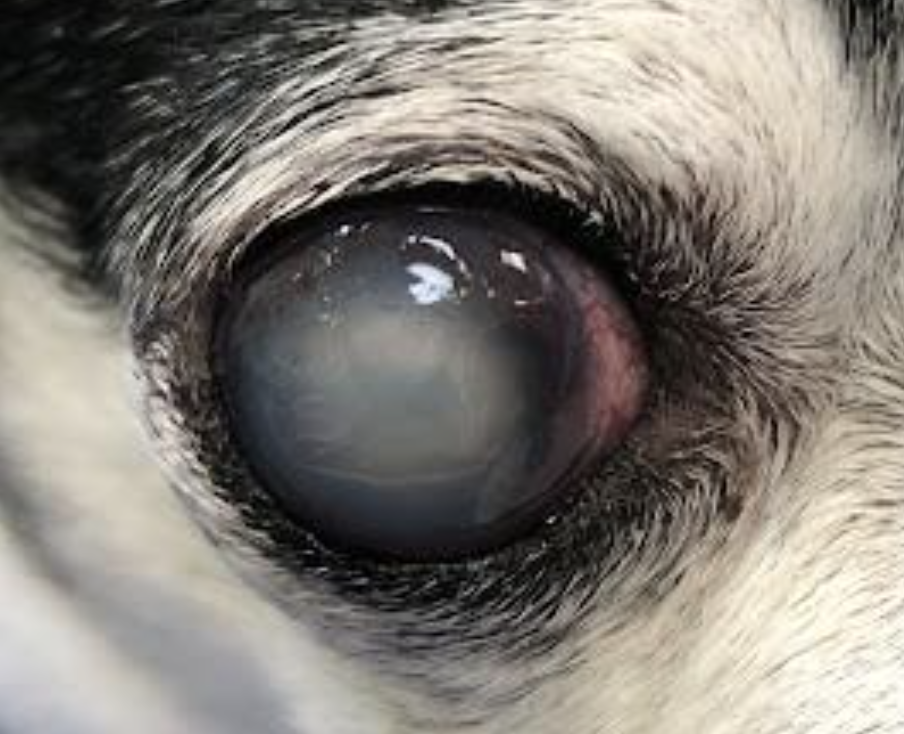
Mature cataracts are complete cataracts where the entire lens (100%) is abnormal and opaque. Vision is significantly reduced to light perception only at this stage. I describe the clinical appearance of mature cataracts to owners as looking like a pearl in the eye.
Hypermature cataracts are starting to breakdown and have passed the mature stage. When talking to clients I typically describe them like a grape shriveling up to a raisin. When this happens the lens proteins leak out of the capsule into the eye causing inflammation. Hypermature cataracts often take on a refractile or glittery appearance clinically and sometimes you may even notice wrinkles within the lens capsule. Many hypermature cataracts imply chronicity however diabetic dogs can reach hypermaturity quickly due to the rapid nature of their development.
Sequelae of Hypermature Cataracts
Lens induced uveitis is the term for inflammation within the eye caused by the lens. This occurs commonly in diabetic cataracts as the osmotic cataract swells and in some cases the lens capsule may even rupture. When this occurs, significant uveitis occurs due to spillage of lens material previously sequestered in the lens capsule into the eye resulting in a foreign body-like attack on the lens material. This can be devastating within an eye resulting in synechia, retinal detachment and glaucoma and preventing the ability to restore vision successfully with surgery.
Hypermature cataracts can also result in lens instability. Chronic uveitis results in disruption of the zonular ligaments that suspend then lens within the eye. Lens capsule contraction can also result in breakage of the ligaments and secondary lens instability. Instability of the lens or luxation can result in development of secondary glaucoma or retinal detachment.
What is the treatment for diabetic cataracts?
Phacoemulsification is the term for cataract surgery, and it is the only way to restore vision in dogs with vision limiting cataracts. Phacoemulsification involves making a corneal incision at the limbus to enter the anterior chamber. Access to the lens is possible after creation of a surgical hole in the lens capsule (capsulorrhexis). Liquification of the lens via high frequency ultrasound followed by replacement of the lens with an artificial or prosthetic lens restores clarity and vision. The incision is closed with 8 or 9-0 suture often in a continuous pattern. Vision is typically significantly improved immediately post-operatively and improves even further over the first several days.
When is the ideal time for surgery and when should these cases be referred?
Ideally phacoemulsification is pursued in the immature to mature stage before lens induced uveitis is a concern. This provides the best possible surgical outcome with the least incidence of post-surgical complications. Hypermature cataracts can often still be successfully treated surgically however the risk of post-operative complications does increase with hypermaturity.
I recommend that patients be referred for evaluation as soon as possible after their diagnosis of diabetes or at least when the initially symptoms of cloudiness or vision loss begin. If an owner is interested in pursuing cataract surgery, seeing the patient early to discuss surgical planning is ideal. Even if owners are not interested in surgery, evaluation by an ophthalmologist may be beneficial to discuss what to expect and to determine if any preventative treatment for sequelae of chronic cataracts would be beneficial.
What can I do for my patients once cataracts are diagnosed?
Our goal is to prevent lens induced uveitis. We typically start patients, especially the diabetic patients, on topical anti-inflammatory drops. Steroids like Prednisolone Acetate or nonsteroidals like Ketorolac, Diclofenac or Flurbiprofen are good choices once the cataracts have been documented to prevent inflammation. These drops are initiated prior to phacoemulsification surgery but are also helpful in non-surgical patients long-term.
If patients are not candidates for surgery the goal is primarily comfort and long-term monitoring for uveitis and glaucoma and treatment when needed becomes the priority.